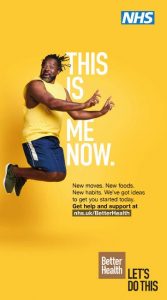
On Monday 27th July, Public Health England is launching a major new adult health campaign to seize the opportunity for a national reset moment of health.
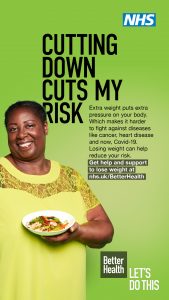
Nearly two thirds (63%) of adults in the UK are overweight or living with obesity. Gaining weight is often a gradual process that takes place over a number of years and modern life doesn’t always make it easy. But this extra weight causes pressure to build up around vital organs, making it harder for the body to fight against diseases like cancer, heart disease and now COVID-19.
By reducing your weight within a healthy range, you can cut your risk of being critically ill with COVID-19. To improve health and wellbeing, individuals should aim to have a BMI below 25 and above 18.52. NICE recommends that Black, Asian and minority ethnic groups (BAME) should aim to have a BMI below 23 and above 18.5 to avoid risks to health.
To support people to live healthier lives, Public Health England’s Better Health campaign will provide a variety of tools and apps to help you make healthier food choices, become more active and prevent future weight gain. One of these tools is a Weight Loss Plan app, which provides 12 weeks worth of engaging content that can be personalised and tailored to the goals and needs of the individual. Later down the line, support will also be made available to help people quit smoking, cut down their drinking and look after their mental health.
For help and support to lose weight, visit www.nhs.uk/BetterHealth
NHS Weight Loss Plan mobile phone app available for iOS and Android
PRIMARY KEY MESSAGES
- Better Health is a ground-breaking new adult health campaign that provides an opportunity for the nation to reset and introduce healthy changes. For many, the past few months have been a wake-up call, with people realising how precious their health is and recognising that it is time to get back on track
- Nearly two thirds of adults in the UK are overweight or living with obesity
- Most people gain weight gradually over a long period of time and modern life doesn’t always make it easy
- Extra weight causes pressure to build up around our vital organs making it more difficult for the lungs to get oxygen around the body
- Extra weight can make it harder for us to fight against diseases like cancer, heart disease and COVID-19
- People living with obesity are twice as likely to be hospitalised with COVID-19
- COVID-19 patients with obesity are more likely to be admitted to intensive care, require advanced treatment and potentially have poorer outcomes, including mortality
- To be a healthy weight, you should aim to have a BMI below 25 and above 18.5. NICE recommends that Black, Asian and minority ethnic groups (BAME) should aim to have a BMI below 23 and above 18.5 to reduce risk to health
- Lowering your BMI helps lower your risk of diseases like cancer, heart disease and now COVID-19
- Public Health England has launched the Better Health campaign to support people to live healthier lives. Better Health has a range of tools to help you make changes to improve your health, including the new 12 Week Weight Loss Plan app, to support people on their weight loss journey
- For help and support to lose weight, visit www.nhs.uk/BetterHealth
SECONDARY KEY MESSAGES (NUTRITION) - If you’re trying to lose weight: for a man aim for a maximum of 400 calories at breakfast and 600 for lunch and dinner (plus drinks and a couple of healthy veg and fruit-based snacks in-between). For women this is around 300 calories at breakfast and 400 at lunch and dinner.
- Try to aim for around 1,400kcals a day if you’re a woman and around 1,900kcals if you’re a man.
- Snack less – no more than twice a day – and go for veg based ones. If you’re having packaged snacks go for those with around 100kcals and stick to two a day max.
- Check the ‘traffic light’ labels and go for foods and drinks with more greens and ambers and less reds.
- When it comes to fruit and veg; the more the better! Get your 5 A Day. They’re low in calories.
SECONDARY KEY MESSAGES (PHYSICAL ACTIVITY) - When it comes to exercise, some is good, but more is better – the more time active you are, the greater the health benefits. Remember every minute counts!
- It is never too late to get active to improve your health, so start small and build up starting from minutes of brisk walking a day
FACTS AND STATS
- Overweight and obesity stats
- Six in 10 (63%) adults in England are above a healthy weight, with 36% of adults being overweight and 27% living with obesity
- Almost seven out of 10 men are overweight or living with obesity (67%) and six out of 10 women are overweight or living with obesity (60%)
- One out of four men is living with obesity (26%) and almost one out of three women is living with obesity (29%)
- 76% of men aged 45-54 years are overweight or living with obesity, this increases to 82% for men aged 55-64 years
- 64% of women aged 45-54 years are overweight or living with obesity, this increases to 66% for women aged 55-64 years
- 34% of men and 48% of women have a very high waist measurement, indicating central obesity
- 2% of men and 4% of women are living with severe obesity (BMI ≥40kg/m2)
- Since 1993-95 the prevalence of severe obesity has risen 7-fold for men (0.3% to 2.1%) and 2.9-fold for women (1.5% to 4.3%)
Prevalence of overweight and obesity in BAME groups - The Active Lives Survey (2017/18) found that approximately 73% of Black adults were living with obesity, compared to 63% white British adults and 57% Asian adults
- Health Survey for England data indicates that 8.3% of Black females are morbidly obese compared to 4% of White females. For men, the prevalence amongst White and Black men is similar 2.4% and 2.3% respectively
Physical Activity - Over 1 in 3 (34%) men and almost half (42%) of women are not active enough for good health, by not doing at least 150 minutes of moderate intensity activity each week
- People in lower socioeconomic groups are more likely to not be active enough for their health, with half (50%) of the most deprived 20% of the population not achieving guidelines compared to around 1 in 3 (32%) of the least deprived 20% (based on quintiles of Index of Multiple Deprivation)
- Physical activity declines with age, with over 2 in 3 (67%) adults aged 19 to 64 years achieving 150 minutes of moderate intensity physical activity per week compared to less than half (44%) of adults aged 65 and over
Health harms - Obesity reduces life expectancy by an average of 4.2 years for men and 3.5 years for women
- 90% of adults with type 2 diabetes aged 16-54 years are overweight or living with obesity
- In England, adults living with obesity are 5 times more likely to be diagnosed with type 2 diabetes than those who are a healthy weight (a body mass index between 18.5 and 25)
- 43% of adults aged 16 and over had at least one longstanding medical condition
- More than half of adults (56%) are at increased, high or very high risk of chronic disease due to their waist circumference and BMI
- In the Global Burden of Disease Study (GBD) 2016, obesity and smoking were the leading risk factors for morbidity. Analysis of the study demonstrated that these are associated with many of the most
- common causes of death including cardiovascular disease, musculoskeletal conditions, respiratory disease, diabetes and most cancers
COVID-19 - People living with obesity are twice as likely to be hospitalised with COVID-19
- Current evidence suggests that COVID-19 patients living with obesity, and in particular morbid obesity, may be more likely to be admitted to intensive care; require advanced treatment; and potentially have poorer outcomes, including greater risk of mortality
- Data from intensive care audit weekly reports, which detail adult intensive care, indicates that 7% of those in intensive care are morbidly obese – this is twice the rates of morbid obesity in the population as a whole
- An NHSE report on diabetes and COVID-19 found that deaths in people with diabetes in England have more than doubled during the COVID-19 epidemic
- The same report found that hyperglycaemia and obesity in both Type 1 and Type 2 diabetes were independently associated with increased COVID-19 mortality. It was also found that risk factor control could reduce the impact of COVID-19 in diabetes
- The OpenSAFELY report, which looked into factors associated with COVID-19-related hospital death in the records of 17 million adult NHS patients, found that most comorbidities studied were associated with increased risk of COVID-19, including cardiovascular disease, diabetes, respiratory disease including asthma, obesity, history of aematological malignancy or recent other cancer, kidney, liver, neurological and autoimmune conditions
- International studies have found that obesity-related conditions seem to worsen the effect of COVID19; the Centres for Disease Control and Prevention (CDC) reported that people with heart disease and diabetes are at higher risk of COVID-19 complications
- The largest number of patients in critical care are from age groups between 50 and 70 for both males and females, and only small numbers aged over 80. When compared to all-cause mortality in previous years, deaths from COVID-19 have a slightly older age distribution, particularly for males
- Between the ages of 40 to 79, the age specific death rates from COVID-19 among males were around double the rates in females compared with 1.5 times for all causes mortality in previous years
- An analysis of survival among confirmed COVID-19 cases shows that, after accounting for the effect of sex, age, deprivation and region, people of Bangladeshi ethnicity had around twice the risk of death when compared to people of White British ethnicity. People of Chinese, Indian, Pakistani, Other Asian, Caribbean and Other Black ethnicity had between 10 and 50% higher risk of death when compared to White British