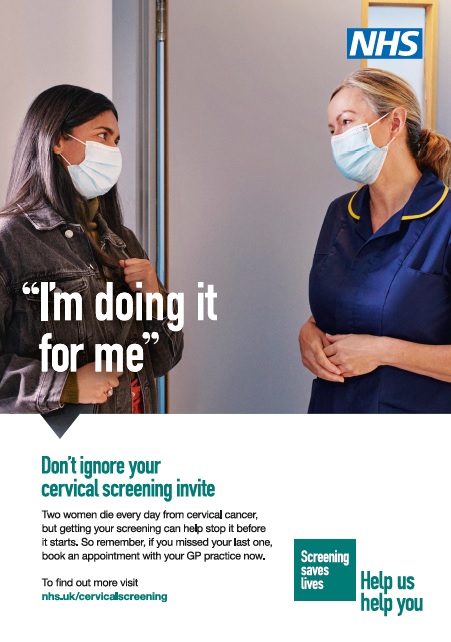
On 14th February 2022, the Office for Health Improvement and Disparities (OHID), with the support of NHS England and NHS Improvement, will launch a national cervical screening campaign. The Help Us Help You – Cervical Screening campaign will encourage those eligible for screening – women and people with a cervix aged 25-64 – to respond to their cervical screening invitation letter, and to book an appointment with their GP practice or sexual health clinic if they missed their last screening.
Two women die every day from cervical cancer, yet it is one of the most preventable cancers. Around 2,700 women in England are diagnosed with cervical cancer each year and it is the second most common cancer amongst women under 35.
The campaign will raise awareness of the risks of cervical cancer and highlight the preventative benefits of screening. The overall aim of the campaign is to increase the number of those eligible to attend their screening.
The key objectives of the campaign are to empower women and people with a cervix to attend their cervical screening. This will be done by communicating the importance and preventative purpose of screening and addressing the specific barriers to screening by providing reassurance, addressing misconceptions and increasing motivation to book an appointment when invited.
Running throughout England for four weeks between 14 February – 14 March 2022, the campaign will include advertising on TV, video on demand, social media and paid search, along with national and regional PR activity. There will also be activity targeted to ethnic minority (Black and South Asian) and LGBTQ+ people with a cervix, as these groups can experience specific barriers to taking up screening.
Our partners play an integral part in supporting this campaign. Local authorities, NHS and NGO partners will be able to order and download digital and print assets from the Campaign Resource Centre (CRC).
Key Messages
Primary messages:
- Two women die every day from cervical cancer in England, yet it is one of the most preventable cancers and getting your screening can help stop it before it starts.
- Screening helps prevent cervical cancer by checking for a virus called high-risk HPV which causes nearly all cervical cancers. This is the best way to find out who is at higher risk of developing the cervical cell changes that over time could potentially lead to cervical cancer. Any cervical cell changes can be treated, preventing cervical cancer.
- But don’t be alarmed if you have HPV as it does not mean you have cervical cancer – HPV is a common virus that most people will get at some point during their lives.
- Women and people with a cervix aged 25-64 are eligible for screening. Those registered as female with their GP practice are invited for routine screening every three years if they are aged 25-49 and every five years if they are aged 50-64. Those registered as male will need to request an appointment from their GP or a local sexual health clinic.
- Life can be hectic and it’s easy to let your cervical screening appointment fall to the bottom of your ‘to do’ list, but it only lasts a few minutes – it’s a few minutes that could save your life.
- For most women and people with a cervix, cervical screening tests are not painful. However, if you are worried that you may find the test uncomfortable, remember you are in control and can ask to stop at any time. If you are worried about it being uncomfortable, or you have found screening difficult in the past, talk to the nurse or doctor doing the test so they can give you the right support.
- If you’re embarrassed about cervical screening then you’re not alone. Talk to the nurse or doctor doing the test, who can help put you at ease.
- During COVID-19 your GP practice remains open and will offer cervical screening appointments. They have put in place safety measures to keep you safe during your cervical screening appointment.
Secondary messages:
- Cervical screening is not a test for cancer. It helps prevent cervical cancer by checking for high-risk Human Papillomavirus (HPV) which causes nearly all cervical cancers. It means any cervical cell abnormalities can be treated. If left untreated, these cells can develop into cancer.
- Your cervical screening sample is first tested for high-risk HPV. HPV testing is more sensitive and accurate than the previous screening method and is the best way to find out who is at higher risk of developing the cervical cell changes that over time could potentially lead to cervical cancer.
- HPV is present on the skin, so it is easy to get and difficult to completely protect against.
- HPV can stay in the body for many years. It can stay at very low or undetectable levels and not cause any problems. However, sometimes it can cause abnormal cells in your cervix to develop. These can, over time, turn into cancer if left untreated
- The symptoms of cervical cancer are not always obvious, and it may not cause any symptoms at all until it’s reached an advanced stage. That’s why it’s important that you attend all your cervical screening appointments.
- The HPV vaccine protects against the most common types of HPV that cause cervical cancer. However, even if you’ve been vaccinated it’s important that you attend your cervical screening appointment because the HPV vaccine doesn’t prevent all cervical cancers.
Call to action(s):
- Cervical screening saves lives – don’t ignore your cervical screening invite and if you missed your last one book an appointment with your GP practice or local sexual health clinic.
- Encourage those you love to get screened if they are overdue a test.
- For further information please visit: www.nhs.uk/cervicalscreening
Facts and statistics
Cervical screening
- People between the ages of 25 and 64 are invited for regular cervical screening under the NHS Cervical Screening Programme. Those registered as female with their GP practice and aged 25 to 49 are invited for routine screening every 3 years. Those registered as female with their GP practice and aged 50 to 64 are invited for routine screening every 5 years.[1] The first invitation for screening is sent at 24.5 years.
- NHS Cervical Screening saves thousands of lives a year in the UK.[2]
- It has been estimated that in England cervical screening prevents 70% of cervical cancer deaths and that if everyone attended screening regularly, 83% of cervical cancer deaths could be prevented.[3]
- On 31st March 2021, 70.2% of eligible individuals had taken up the offer of screening *. This has decreased from 72.2% on 31 March 2020.[4]
- The expected national standard for cervical screening coverage is 80% for eligible individuals. At March 2021 no region or local authority met this threshold. 91 out of 149 local authorities had coverage levels of 70% and above, a decrease of 12 compared to 2020.4
- Cervical screening coverage in the older age group (50-64 years) is consistently higher than the younger age group (25-49 years):
- 68% of those aged 25 – 49 were screened* at 31st March 2021, compared to 70.2% in 20204
- 74.7% of those aged 50 – 64 were screened* at 31st March 2021, compared with 76.1% at 31st March 20204
- Cervical screening coverage has declined by 5.5% in the last 10 years.[5] At 31st March 2011 75.7% of those eligible were screened, dropping to 71.4% at 31st March 2018. Screening coverage rose in 2019 (71.9%) and 2020 (72.2%) but fell again to 70.2% at 31st March 2021, probably due to the impact on screening of the COVID-19 lockdown.
- Over the past 10 years, screening* has declined by 5.4% in the older age group (since 31 March 2011) and declined by 5.8 % in the younger age group.5
- Those aged 25-29 are least likely to take up their cervical screening invitation but have a higher rate of abnormality detected in screening compared to other age groups.5
- 3.03 million individuals aged 25 to 64 were tested in 2020 – 2021.4
- 4.59 individuals aged 25 to 64 were invited for screening in 2020–21.4
- The results from the 2019 Cervical Screening campaign show that there were 86,000 more screening tests carried out during the campaign period than in the same period the year before.[6]
- High-risk HPV DNA is found in over 99% of cervical cancer cases.[7]
HPV Vaccine
- Cervical cancer rates are almost 90% lower in women vaccinated against HPV.[8]
- Studies have shown that the vaccine protects against HPV infection for at least 10 years, although experts expect protection to last for much longer. But because the HPV vaccine does not protect against all types of HPV that can cause cervical cancer, it’s important that all those with a cervix who receive the HPV vaccine also have regular cervical screening once they reach the age of 25.
Ethnic Minority
- A survey commissioned by Jo’s Trust found that ethnic minority women of screening age were more likely than white women to say they had never attended a cervical screening (12% vs 8%). 30% of Asian women reported not knowing what cervical screening is.[9]
- Poor understanding of what the test was for and why it was important has been highlighted as a barrier to cervical screening, with twice as many ethnic minority women (30%) as white women (14%) saying that better knowledge about the test and its importance would encourage them to attend the screening.9
Risk factors
- Most cases of cervical cancer are caused by Human Papillomavirus (HPV) which is a common virus that 4 out of 5 (80%) of us will have at some point during our lives.
- HPV spreads through close skin-to-skin contact of the genital area, not just from penetrative sex. This includes vaginal, oral or anal sex; any skin-to-skin contact of the genital area; sharing sex toys. It can stay at very low or undetectable levels and not cause any problems. This means an HPV infection may have come from a partner a long time ago.
Cervical cancer incidence
- Around 2,700 women are diagnosed with cervical cancer each year in England.[10]
- Seven women are diagnosed with cervical cancer every day in England.10
- Cervical cancer is the 11th most common cancer in women in England10
- The latest annual data shows that cervical cancer is the second most common cancer among women under the age of 35 in England.10
Cervical cancer mortality
- Around 690 women die from cervical cancer each year in England.10
- Two women die every day from cervical cancer in England10
Changes in incidence and mortality over time
- Since the early 1990s, cervical cancer incidence rates have decreased by a quarter (25%) in women in the UK (2016 – 2018).[11]
- Since the early 1970s, cervical cancer mortality rates have decreased by three-quarters (75%) in women in the UK.[12]
England comparison to Europe
- The survival rate for women with cervical cancer in England is below Europe. Latest data shows the five-year survival in Europe was 62.4% (2000-2007) compared with 61.2% (2014-2018) for England.[13]
Ethnic Minority Activity:
A range of targeted activity will take place to initiate conversations about screening and tackle the cultural barriers. This will include:
- Paid editorial activity featuring films with Black and South Asian women talking to a media medic about cervical screening, running across ethnic TV and radio stations and social media.
- PR activity utilising case studies, healthcare professionals and well-known celebrities and influencers from Black and South Asian communities.
- Black and South Asian social media groups (Facebook, Instagram and Twitter) and podcasters creating compelling content for their followers
Activity for Disabled People:
Disabled women and people with a cervix, particularly those with sensory impairments including BSL users, are likely to experience barriers to accessing mainstream communications and steps have been taken to reach these audiences. People with a learning disability are a particular focus as they are less likely to be screened.[14]
To reach these audiences campaign assets will be available in alternative formats in:
- BSL versions of TV, social and PR films
- large print, braille, audio versions of posters
- an easy read leaflet
- Cervical screening picture leaflet
Engagement will take place with disability organisations and channels to help reach disabled people, their carers and influencers to encourage and reinforce the communication of messaging and availability of alternative formats.
LGBTQ+ Activity:
Lesbian and bisexual women are less likely to have been for cervical screening. Figures show that 15% of lesbian and bisexual women over 25 have never had a cervical screening test compared to 7% of women over 25 in general.[15]
Trans men and non-binary people with a cervix also experience specific issues and require tailored messages.[16] Trans men and non-binary people with a cervix aged 25-64 are eligible for cervical screening. Those registered as male will not be automatically invited and need to request an appointment from their GP or a local sexual health clinic.
OHID has worked with LGBTQ+ organisations to develop this strand of the campaign. LGBTQ+ influencers have also been recruited to produce tailored, authentic social media content to resonate with their followers.
Key messages for LGBTQ+ audiences
- Women and people with a cervix aged 25-64 are eligible for screening. Those registered as female with their GP practice are invited for routine screening every three years if they are aged 25-49 and every five years if they are aged 50-64. Those registered as male will need to request an appointment from their GP or a local sexual health clinic.
- Trans men and non-binary people with a cervix aged 25-64 are eligible for cervical screening. They can arrange to be screened with their GP practice or a local sexual health clinic.
- If you have a cervix and have had any kind of sexual contact, with people of any gender, you are at risk of cervical cancer.
- Most cases of cervical cancer are caused by Human Papillomavirus (HPV) which is a common virus that most people will get at some point during their lives. This is because HPV is spread through close skin to skin contact during any type of sexual activity.
- You can have HPV even if you’ve only ever had one partner, or not had sex for a long time.
* This refers to screening coverage, which is defined as the percentage of those in a population eligible for screening at a given point in time who were screened adequately within a specified period. For those aged 25-49, the time period is within the last 3.5 years. For those aged 50-64, the time period is within the last 5.5 years.
[1] “Invited for routine screening” refers to those invited through the Screening Programme in 2020/21. The number of those tested includes individuals who had screening tests not prompted by the Screening Programme, eg tests initiated by a nurse with those who are overdue for screening.
[2] NHS cervical screening leaflet. Available from:
https://www.gov.uk/government/publications/cervical-screening-description-in-brief
[3] Landy, R., Pesola F., et al., Impact of cervical screening on cervical cancer mortality: estimation using stage-specific results from a nested case–control study. British Journal of Cancer volume115, pages1140–1146 (25 October 2016). Available from: https://www.nature.com/articles/bjc2016290?foxtrotcallback=true
[4] Cervical Screening Programme England 2020- 2021 https://digital.nhs.uk/data-and-information/publications/statistical/cervical-screening-annual/england—2020-21
[5] Cervical Screening Official Statistics 2020-21 published by NHS Digital https://digital.nhs.uk/data-and-information/publications/statistical/cervical-screening-annual/england—2020-21
* This refers to screening coverage, which is defined as the percentage of women in a population eligible for screening at a given point in time who were screened adequately within a specified period. For those aged 25-49, the time period is within the last 3.5 years. For those aged 50-64, the time period is within the last 5.5 years.
[6] PHE Screening Blog Cervical Screening Saves Lives – highlights from the national campaign – PHE Screening (blog.gov.uk)
[7] 99.8% of cervical cancer cases in the UK are caused by HPV infection” https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/cervical-cancer/risk-factors#ref-2
[8] The Lancet: The effects of the national HPV vaccination programme in England, UK, on cervical cancer and grade 3 cervical intraepithelial neoplasia incidence: a register-based observational study (Date accessed: December 1, 2021) https://doi.org/10.1016/S0140-6736(21)02178-4
[9] YouGov survey. Total sample size was 1179 white women aged 25-65 and 1177 BAME women aged 25-65. Fieldwork was undertaken between 30th June – 7th July 2011. Available from: https://www.jostrust.org.uk/sites/default/files/bme_research_2011_final.pdf bme_research_2011_final.pdf (jostrust.org.uk)
[10] Cancer Registration Statistics, England 2019. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/cancer-registration-statistics/england-2019#summary Data obtained from NCRAS, PHE. On average 2687 women were diagnosed with cervical cancer (ICD-10 C53) each year from 2017 – 2019 and 689 women died from the disease. The latest annual data is for 2019
[11] Cervical cancer incidence statistics, CRUK. Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/cervical-cancer/mortality%20-%20heading-Two#heading-Zero
[12] Cervical cancer mortality statistics, CRUK. Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/cervical-cancer/mortality%20-%20heading-Two#heading-Two
[13] Cervical cancer survival comparisons, CRUK. Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/cervical-cancer/survival#heading-Four
[14] Supporting women with learning disabilities to access cervical screening – GOV.UK (www.gov.uk)
[15] Addressing inequalities in LGBT cancer screening coverage – PHE Screening (blog.gov.uk)
[16] Cervical screening for trans men and/or non-binary people | Jo’s Cervical Cancer Trust (jostrust.org.uk)